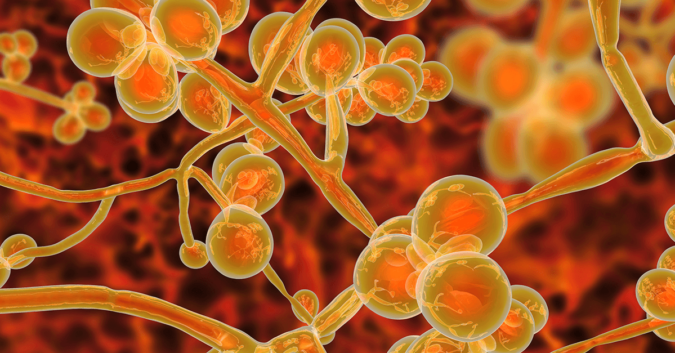
Of the millions of different species of fungi in the world, only about 300 are known to make people sick. Unfortunately, an outbreak of one such deadly fungus is causing severe illness in hospitalized patients around the globe. Though healthy people will likely fight off an infection, the fungus is prevalent in nursing homes and hospitals where patients are most vulnerable.
Candida auris, or C. auris, as the fungus is known, is difficult to identify and hard to eradicate. It can spread quickly, and once a person is infected, the disease can be fatal. The Centers for Disease Control and Prevention (CDC) estimate that 30%-60% of patients with C. auris infections have died.
Some nursing homes have become hotbeds for this fungal infection. Instead of helping people recover, nursing homes are infecting people. Along with the other nursing home red flags, it appears that residents and families need to be aware of the spread of C. auris, which is far from contained.
7 Things to Know about C. auris
1. C. auris Is a Fungus That Can Cause Life-Threatening Infections
C. auris is a species of yeast (which is a type of fungus) that can cause severe illness in hospitalized patients. It was first discovered in 2009, in the ear canal of a female patient in a Japanese hospital. Auris is Latin for ear, but the infection may also affect the blood, heart, brain, eyes, bones, and other parts of the body.
It is much more serious than other Candida infections (candidiasis), which commonly occur in the mouth (thrush) and vagina (yeast infections). Infections caused by C. Auris are known as invasive candidiasis and can be fatal after entering the bloodstream.
2. Nursing Home Residents and Hospitalized Patients Are at Increased Risk
C. auris infections have been found in people of all ages, but those at the highest risk of getting an infection are nursing home residents, especially those in ventilator units or with medical devices that enter their body, such as breathing tubes, feeding tubes, and central venous catheters.
People with weakened immune systems should also be alert, particularly those who have spent time in a healthcare setting, where they have a greater likelihood of encountering the deadly fungi.
3. The C. auris Outbreak Is Worldwide
As of September 11, 2019, the CDC has confirmed 769 cases of C. auris in the United States, spread across 13 states: California, Connecticut, Florida, Georgia, Illinois, Indiana, Maryland, Massachusetts, New Jersey, New York, Oklahoma, Texas, and Virginia.
Hardest hit so far are New York City, Chicago, and their surrounding areas. In addition to confirmed cases, there were 30 probable cases and 1,540 patients carrying the fungi on their body without signs of an active infection.
Cases of C. auris have been documented in 35 other countries. According to the agency, the strains of C. auris in the U.S. were unintentionally brought into American hospitals by patients who had recently received healthcare in India, Kenya, Kuwait, Pakistan, South Africa, the United Arab Emirates, and Venezuela.
4. C. auris Is Hard to Diagnose Correctly
Symptoms of C. auris infection vary greatly and depend on which part of the body is affected — a bloodstream infection presents differently than an ear infection, for example. Typically, patients with C. auris are already sick, which means they have serious conditions that may share or mask symptoms of a C. auris infection.
Even when an infection is recognized, specialized laboratory tests are necessary in order to accurately diagnose C. auris. The CDC has informed healthcare professionals that the normal methods of infection identification can easily lead to a misidentification of C. auris. This can delay proper care for the patient and allow the fungi to spread to others.
5. C. auris Is Multi-Drug Resistant
C. auris is not the only species of Candida to cause infections, but the CDC says that more than 90% of C. auris infections are resistant to at least one antifungal medication, and some have been resistant to all 3 main classes of antifungal medications.
This makes C. auris infections more difficult to manage, though they are treatable with multiple classes of antifungals at high doses. Still, there are a limited number of antifungal medications, and resistant strains raise the prospect of common infections becoming incurable.
6. C. auris Can Spread Quickly in Nursing Homes and Hospitals
As an organism, C. auris is very resilient. According to new research presented in July from the University of Minnesota Center for Infectious Disease Research and Policy, C. auris can survive on dry surfaces for weeks.
In hospitals and nursing homes, it can be extremely difficult to sanitize contaminated rooms and patients. The researchers observed a skilled nursing facility in Chicago that had experienced an outbreak of C. auris. Even after using bleach and special antiseptics, more than 70% of residents tested positive.
7. Dangerous Nursing Homes Raise the Risk of Infection
Because the nursing home patient population is so vulnerable, skilled nursing facilities need to practice rigorous infection control. Unfortunately, nursing homes are often understaffed or unprepared to provide the level of care needed to keep people safe.
A recent New York Times investigation of skilled nursing homes found that they are breeding grounds for the deadly fungus. Lax safety measures can lead to the spread of the fungus within the facility. Then, patients carrying C. auris are sent to hospitals without warning, where they can infect other at-risk patients.
In the New York Times report, the journalist watched staff at one nursing home in New York disregard sanitary protocol multiple times.
Nursing Homes Are Not Supposed to Get People Sick
There are protocols for keeping infection and disease under control — when they are not followed, people get hurt.
For nursing home patients and their families, the threat posed by drug-resistant fungal infection adds to the growing list of concerns. Nursing home abuse and neglect are widespread and inexcusable, but so are the invisible dangers of ignoring safety measures.